Chickenpox

At Sussex Private GP Clinic, we believe prevention is the cornerstone of lifelong health and wellbeing. Vaccinations play a vital role in protecting you and your loved ones from a range of preventable illnesses, helping to safeguard your health both now and in the future. Our private vaccination services provide convenient access to safe and […]
Postnatal service

At Paediatric Diagnostics, we understand the importance of caring for both mother and baby during the vital postnatal period. We are delighted to announce the launch of our new Postnatal Service, which will be available at our newly extended clinic. Our consultant-led service is dedicated to providing exceptional postnatal care, offering comprehensive support to ensure […]
GP consultation

Sussex Private GP Clinic is an integral part of Paediatric Diagnostics, a leading healthcare provider committed to delivering exceptional diagnostic and general medical services for children from birth to 18 years old. Contact us Paediatric Diagnostics was established in direct response to the increasing closure of paediatric services within private hospitals across the UK. We […]
Newborn Service

Welcoming a new baby into the world is an exciting and emotional journey, but it can also come with its share of challenges. At our Newborn Care Service, we offer professional, compassionate support to help you navigate these early months, ensuring your baby’s health and development are on track. From feeding advice and sleep routines […]
Skin Prick Test
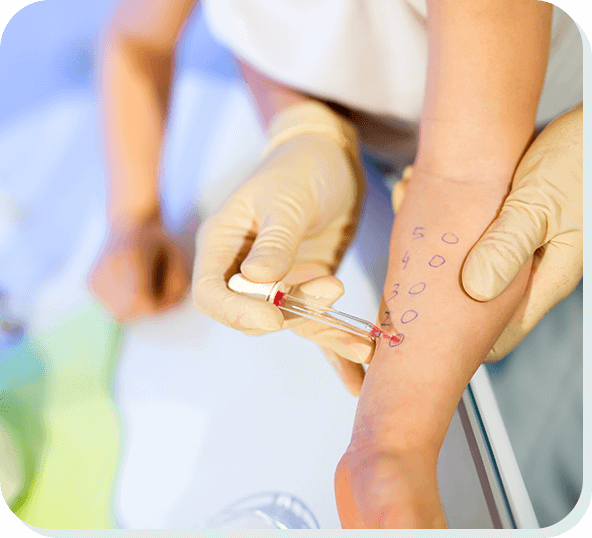
As a parent, ensuring your child’s health and comfort is paramount. One crucial aspect of this is understanding and managing potential allergies. Our expert paediatric nursing staff are here to help with a reliable and efficient diagnostic tool: the skin prick test. We are proud to offer this essential service for babies aged 4 months […]
Video capsule endoscopy

Video capsule endoscopy (VCE) is an advanced diagnostic procedure used to capture wireless images of the small intestine’s inner lining. This technology has become increasingly popular, particularly among paediatric patients. The capsule itself is 24.5mm long and 10.8mm wide and can either be swallowed by older children or introduced using a gastroscope in younger patients. […]
Echocardiogram (ECHO)

At Paediatric Diagnostics, we specialise in delivering top-tier private paediatric echocardiogram services tailored to meet your child’s medical requirements. Our team of skilled paediatric cardiologists is committed to delivering exceptional care, employing advanced imaging technology to accurately diagnose and monitor various heart conditions in children. We are located at Charlwood, West Sussex, making us easily […]
Children’s Gastroenterology Service

Our dedicated paediatric gastroenterology service is committed to the care and well-being of children experiencing a wide array of gastrointestinal and nutritional issues. We provide expert diagnosis, treatment and management for a variety of conditions, including: Abdominal pain Chronic diarrhoea and constipation Coeliac disease Crohn’s disease Feeding difficulties and weight loss Food allergies Gastro-oesophageal reflux […]
Children’s Cardiology Service

Paediatric Diagnostics offers childhood cardiology investigation and treatment for children from birth up to 16 years of age, suffering from cardiology concerns. This includes chest pain, heart murmurs, heart rhythm problems and fainting. Our expert team of private paediatric cardiologists and specialist nurses are highly experienced in providing treatment for children across a wide range […]
Children’s Dermatology Service

At our Specialised Paediatric Dermatology Service, we are profoundly dedicated to the health and well-being of children facing a broad spectrum of dermatology conditions. Our comprehensive services cater to a wide range of skin issues, ensuring that each child receives the highest level of care and attention. We are located at Charlwood, West Sussex, making […]